모던칼럼
근육의 guarding에 관련 한 에릭 달튼 글..( 저자의 허락을 받고 올림니다. 무단 복사 배포 금지)
| Pain – Spasm – Pain by Erik Dalton, Ph.D.
When the brain senses bony instability or tissue damage in-and-around the spine, split decisions are made that help determine the extent of threat to the individual and what actions need to be taken (Fig 1). Layering the area with protective muscle guarding is one such decision. It’s the brain’s reflexogenic attempt to prevent further insult to the injured tissues. By ‘splinting’ the area with spasm, the hypercontracted (shortened) muscles effectively reduce painful joint movements. This is a common source of spasm clinicians address day in and day out… but how does it develop?
Recall that when a joint is moved beyond its acceptable range of motion (physiologic barrier), the facets can become locked open on one side or closed on the other causing loss of joint play (Fig 4). Contrary to popular thinking, the secondary muscle changes that result in the deep groove muscles from joint blockage do not always result in hypertonicity or spasm. Dr. Stuart McGill found that when a lumbar facet joint became displaced and fixated during a lifting incident, the multifidus on the side of the fixated facets began to atrophy within 24 hours (Fig 5). Regardless of the reason for loss of joint play, when vertebrae are not free to move, muscles assigned the job of moving them (prime movers) cannot carry out their duties and are substituted by synergistic stabilizers, i.e., the brain sends in the subs when a key player is injured. The final stage of dysfunction occurs when the middle layer and deep myofascial support systems collapse due to joint dysfunction and the load is shifted to global (outer layer) dynamic muscles such as the erectors, obliques and lats.
To help maintain flexibility, joint capsules require daily or at least frequent elongation to avoid cross-linking of collagen fibers. Articular stretching and myofascial mobilization techniques help therapists restore and maintain capsular elasticity by preventing cross-linking. Long-term joint fixations are a primary cause of reduced flexibility as calcium deposits infiltrate the capsule and associated periarticular structures. As edema collects at the injured site, protein is deposited outside the arterial capillary walls. Soon, chemoreceptors are stimulated and the area becomes a feeding-ground for chemical waste products and accompanying fibrosis. | |
|
Minimizing the accumulation of nociceptive tissue irritants at the injured capsule is the desired result of Myoskeletal mobilization therapy. Adding soft-tissue capsular work not only helps restore range of motion and joint-play to frozen spinal, hip and shoulder articulations, but normalizes afferent messages to the brain; thus reducing protective muscle guarding around the dysfunctional joint. | |


 Much has been written in manual therapy texts about loss of flexibility and range of motion due to fascial contractures, trigger points, ligament fibrosis, spasmodic muscles and the like, with less emphasis placed on the neurology that may be initiating these soft tissue changes. Here are some thoughts on how spinal soft tissues such as joint capsules, facet joints, ligaments, and deep intrinsic (groove) muscles decompensate causing altered movement patterns and pain-generating cycles.
Much has been written in manual therapy texts about loss of flexibility and range of motion due to fascial contractures, trigger points, ligament fibrosis, spasmodic muscles and the like, with less emphasis placed on the neurology that may be initiating these soft tissue changes. Here are some thoughts on how spinal soft tissues such as joint capsules, facet joints, ligaments, and deep intrinsic (groove) muscles decompensate causing altered movement patterns and pain-generating cycles. Here’s a common example: The client comes in complaining of ‘stabbing’ back spasm following a bending and twisting incident apparently due to sudden asymmetrical spinal loading (Fig 2). If there is poor intrinsic and extrinsic myofascial balance and instability, the deepest spinal layer (osteoligamentous canal) may suffer damage. In the presence of joint dysfunction, i.e., facets locked open or closed, ligament strain, etc., the brain senses weakness via mechanoreceptors. The deep spinal groove muscles (rotatores, multifidus and intertransversarii, etc.) are the first tissues reflexively affected by the motion-restricted joint.
Here’s a common example: The client comes in complaining of ‘stabbing’ back spasm following a bending and twisting incident apparently due to sudden asymmetrical spinal loading (Fig 2). If there is poor intrinsic and extrinsic myofascial balance and instability, the deepest spinal layer (osteoligamentous canal) may suffer damage. In the presence of joint dysfunction, i.e., facets locked open or closed, ligament strain, etc., the brain senses weakness via mechanoreceptors. The deep spinal groove muscles (rotatores, multifidus and intertransversarii, etc.) are the first tissues reflexively affected by the motion-restricted joint.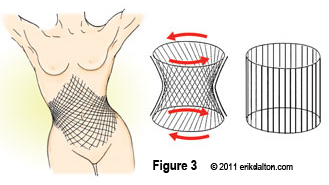 Micro or macro trauma can neurologically inhibit or weaken these deepest spinal layers causing the brain to call for help from middle layer (core) stabilizers such as the QL, psoas, and transverse abdominis (Fig 3). Unfortunately, the middle layer core support system is designed for stabilization to allow global (extrinsic) muscles and fascia to carry out movements of daily life. When they’re called in to “sub” for weak spinal groove muscles and ligaments, it can alter firing order and activation patterns. Prolonged joint fixation leads to aberrant movement and postural patterns which, in time, can be relearned as normal (neuroplasticity).
Micro or macro trauma can neurologically inhibit or weaken these deepest spinal layers causing the brain to call for help from middle layer (core) stabilizers such as the QL, psoas, and transverse abdominis (Fig 3). Unfortunately, the middle layer core support system is designed for stabilization to allow global (extrinsic) muscles and fascia to carry out movements of daily life. When they’re called in to “sub” for weak spinal groove muscles and ligaments, it can alter firing order and activation patterns. Prolonged joint fixation leads to aberrant movement and postural patterns which, in time, can be relearned as normal (neuroplasticity).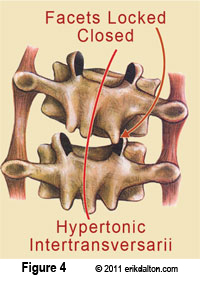 Due to the population’s general lack of proper core support and our inability to adequately activate the middle layer, the intrinsic postural muscles (that burn oxygen for fuel) many times can’t “hold on” long enough to allow for proper mobilization and the load falls back to the damaged joint capsules, spinal ligaments and articular facets.
Due to the population’s general lack of proper core support and our inability to adequately activate the middle layer, the intrinsic postural muscles (that burn oxygen for fuel) many times can’t “hold on” long enough to allow for proper mobilization and the load falls back to the damaged joint capsules, spinal ligaments and articular facets.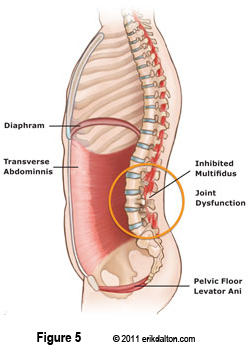 Spasm develops as tissues designed for movement are forced to act both as movers and stabilizers. These fast-twitch muscles provide bursts of energy and do not respond well to compressional loading and soon give out. This is why we commonly see thickened ropes of erector spinae spasm on the ipsilateral side of the joint dysfunction. Longissimus, iliocostalis and the thoracolumbar fascia are forced to carry the load meant for the deep and middle core stabilizers. When these glucose burning tissues tire and spasm, the lubricating fluid between fascial bags begins to dehydrate and the facial envelops adhere to neighboring structures often causing the big ‘wad’ of hypertrophied tissue that therapist’s beat on session-after-session.
Spasm develops as tissues designed for movement are forced to act both as movers and stabilizers. These fast-twitch muscles provide bursts of energy and do not respond well to compressional loading and soon give out. This is why we commonly see thickened ropes of erector spinae spasm on the ipsilateral side of the joint dysfunction. Longissimus, iliocostalis and the thoracolumbar fascia are forced to carry the load meant for the deep and middle core stabilizers. When these glucose burning tissues tire and spasm, the lubricating fluid between fascial bags begins to dehydrate and the facial envelops adhere to neighboring structures often causing the big ‘wad’ of hypertrophied tissue that therapist’s beat on session-after-session.

